Over the last several weeks healthcare, in general, has changed. Providers are closing their doors, patients are waiting in their cars to be seen, and telemedicine is the new buzz word.
How do we navigate this new terrain?
- Breathe: There is so much information floating around it is difficult to find the one piece you need to get going. We are here to help you in this new adventure and will walk in lockstep with you.
- Embrace what you can: Telemedicine isn’t for everyone, but it might be for you. Let’s take a clear look at what telemedicine really means and how you might use it in your office.
- Ask for help: MedNetworx is here to help you. We want to make sure every office has the chance to stay open and even more so, keep that revenue stream flowing.
Telehealth
We have compiled this information over the last several weeks and it is current as of this posting. Please note that some information may change as CMS and other payers release new policies.
What is telehealth?
Telehealth, telemedicine and related terms generally refer to providing care services at-a-distance.
Why has this changed?
Center for Medicare & Medicaid Services (CMS) has expanded this benefit due to the current circumstances. This includes the expanded use of telehealth to help those who need routine care while limiting exposure to other patients.
What do I do?
This is a good question. Analyze your practice’s needs. Can you see patients remotely? Are there certain things you can do with a telephone call to avoid a face-to-face encounter? Do you feel that you can provide care remotely? Each provider answers these questions differently, but be sure you check with your medical association/society to see what they say. ACOG, AAFP, AAOS, AAO, etc. have statements regarding telemedicine.
How do I do this?
We can help!
Find technology that works for you and your patients.
Consider applications that are easy for patients to use and can be used from a cell phone, iPad, and/or computer. AMA has a great quick guide to implementing telemedicine in your practice. HHS sent out their Notification of Enforcement Discretion for Telehealth Remove Communications during the COVID-19 Nationwide Public Health Emergency on March 17, 2020. This brings up the question of what technology to use to conduct these telehealth visits. Below is a portion of the article.
Under this Notice, covered health care providers may use popular applications that allow for video chats, including Apple FaceTime, Facebook Messenger video chat, Google Hangouts video, or Skype, to provide telehealth without risk that OCR might seek to impose a penalty for noncompliance with the HIPAA Rules related to the good faith provision of telehealth during the COVID-19 nationwide public health emergency. Providers are encouraged to notify patients that these third-party applications potentially introduce privacy risks, and providers should enable all available encryption and privacy modes when using such applications.
Under this Notice, however, Facebook Live, Twitch, TikTok, and similar video communication applications are public facing, and should not be used in the provision of telehealth by covered health care providers.
Covered health care providers that seek additional privacy protections for telehealth while using video communication products should provide such services through technology vendors that are HIPAA compliant and will enter into HIPAA business associate agreements (BAAs) in connection with the provision of their video communication products. The list below includes some vendors that represent that they provide HIPAA-compliant video communication products and that they will enter into a HIPAA BAA.
- Skype for Business
- Updox
- VSee
- **Zoom for Healthcare
- Doxy.me
- Google G Suite Hangouts Meet
Note: OCR has not reviewed the BAAs offered by these vendors, and this list does not constitute an endorsement, certification, or recommendation of specific technology, software, applications, or products. There may be other technology vendors that offer HIPAA-compliant video communication products that will enter into a HIPAA BAA with a covered entity. Further, OCR does not endorse any of the applications that allow for video chats listed above.
Under this Notice, however, OCR will not impose penalties against covered health care providers for the lack of a BAA with video communication vendors or any other noncompliance with the HIPAA Rules that relates to the good faith provision of telehealth services during the COVID-19 nationwide public health emergency.
Review the documentation guidelines
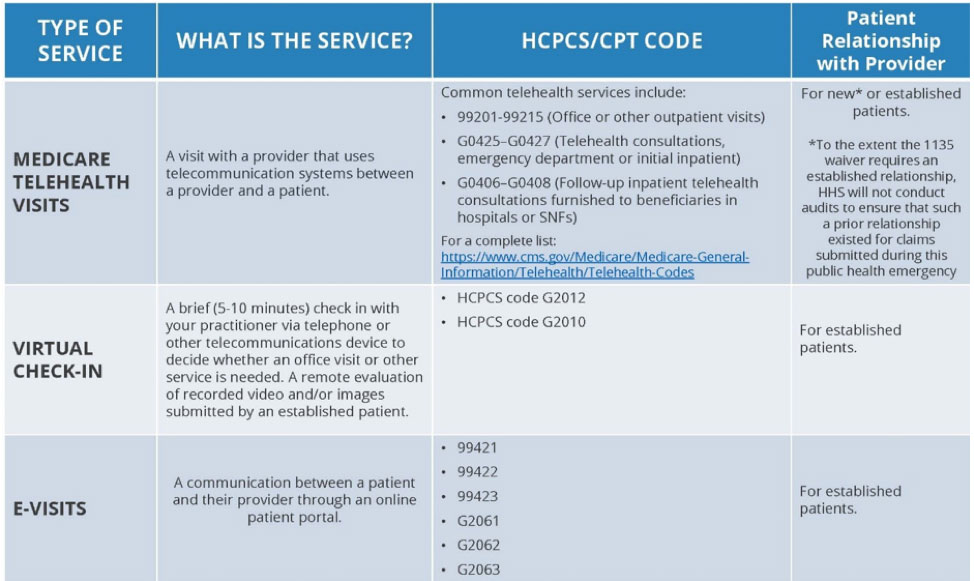
The best documentation for this is from CMS. The fact sheet is concise and easy to read. You can also review the CMS telehealth toolkit. Below is some of the information included:
Update your business/biller/officer manager
Now that you’ve decided to provide care remotely, your business office will need to know how to send the claims. Each payer has proven to be a little different, but below are CMS’ answers to the most frequently asked questions. Reach out to your payers to find their specific guidelines.
Invite your patients to participate.
When reminding your patients of their upcoming appointment, offer them the choice of an office visit or telehealth visit. The patient needs to approve the telehealth interaction before you invite them to a telehealth visit.
Medicare Telehealth Frequently Asked Questions (FAQs)
March 17, 2020
1. Q: How will recently enacted legislation allow CMS to utilize Medicare telehealth to address the declared Coronavirus (COVID-19) public health emergency?
A: The Coronavirus Preparedness and Response Supplemental Appropriations Act, as signed into law by the President on March 6, 2020, includes a provision allowing the Secretary of the Department of Health and Human Services to waive certain Medicare telehealth payment requirements during the Public Health Emergency (PHE) declared by the Secretary of Health and Human Services January 31, 2020 to allow beneficiaries in all areas of the country to receive telehealth services, including at their home.
2. Q: What does this mean? What payment requirements for Medicare telehealth services are affected by the waiver?
A: Under the waiver, limitations on where Medicare patients are eligible for telehealth will be removed during the emergency. In particular, patients outside of rural areas, and patients in their homes will be eligible for telehealth services, effective for services starting March 6, 2020.
3. Q: Why wasn’t this done before?
A: Current telehealth law only allows Medicare to pay practitioners for services like routine visits furnished through telehealth under certain circumstances. For example, the beneficiary receiving those services must generally be located in a rural area and in a medical facility. Where the beneficiary receives those services is known as the “eligible originating site.” The beneficiary’s home is generally not an eligible originating site, but under the new 1135 waiver, this will be waived during the emergency. This will now allow telehealth services to be provided in all settings –including at a patient’s home.
4. Q: What services can be provided by telehealth under the new emergency declaration?
A: CMS maintains a list of services that are normally furnished in-person that may be furnished via Medicare telehealth. This list is available here: https://www.cms.gov/Medicare/Medicare-GeneralInformation/Telehealth/Telehealth-Codes. These services are described by HCPCS codes and paid under the Physician Fee Schedule. Under the emergency declaration and waivers, these services may be provided to patients by professionals regardless of patient location.
5. Q: Would physicians and other Qualified Providers be able to furnish Medicare telehealth services to beneficiaries in their homes?
A: Yes. The waiver temporarily eliminates the requirement that the originating site must be a physician’s office or other authorized healthcare facility and allows Medicare to pay for telehealth services when beneficiaries are in their homes or any setting of care.
6. Q: Who are the Qualified Providers who are permitted to furnish these telehealth services under the new law?
A: Qualified providers who are permitted to furnish Medicare telehealth services during the Public Health Emergency include physicians and certain non-physician practitioners such as nurse practitioners, physician assistants and certified nurse midwives. Other practitioners, such as certified nurse anesthetists, licensed clinical social workers, clinical psychologists, and registered dietitians or nutrition professionals may also furnish services within their scope of practice and consistent with Medicare benefit rules that apply to all services. This is not changed by the waiver.
7. Q: Will CMS enforce an established relationship requirement?
A: No. It is imperative during this public health emergency that patients avoid travel, when possible, to physicians’ offices, clinics, hospitals, or other health care facilities where they could risk their own or others’ exposure to further illness. Accordingly, the Department of Health and Human Services (HHS) is announcing a policy of enforcement discretion for Medicare telehealth services furnished pursuant to the waiver under section 1135(b)(8) of the Act. To the extent the waiver (section 1135(g)(3)) requires that the patient have a prior established relationship with a particular practitioner, HHS will not conduct audits to ensure that such a prior relationship existed for claims submitted during this public health emergency.
8. Q: Is any specialized equipment needed to furnish Medicare telehealth services under the new law?
A: Currently, CMS allows for use of telecommunications technology that have audio and video capabilities that are used for two-way, real-time interactive communication. For example, to the extent that many mobile computing devices have audio and video capabilities that may be used for two-way, real-time interactive communication they qualify as acceptable technology. The new waiver in Section 1135(b) of the Social Security Act explicitly allows the Secretary to authorize use of telephones that have audio and video capabilities for the furnishing of Medicare telehealth services during the COVID-19 PHE. In addition, effective immediately, the HHS Office for Civil Rights (OCR) will exercise enforcement discretion and waive penalties for HIPAA violations against health care providers that serve patients in good faith through everyday communications technologies, such as FaceTime or Skype, during the COVID-19 nationwide public health emergency. For more information, click here.
9. Q: How does a qualified provider bill for telehealth services?
A: Medicare telehealth services are generally billed as if the service had been furnished in-person. For Medicare telehealth services, the claim should reflect the designated Place of Service (POS) code 02-Telehealth, to indicate the billed service was furnished as a professional telehealth service from a distant site.
10. Q: How much does Medicare pay for telehealth services?
A: Medicare pays the same amount for telehealth services as it would if the service were furnished in person. For services that have different rates in the office versus the facility (the site of service payment differential), Medicare uses the facility payment rate when services are furnished via telehealth.
11. Q: Are there beneficiary out of pocket costs for telehealth services?
A: The use of telehealth does not change the out of pocket costs for beneficiaries with Original Medicare. Beneficiaries are generally liable for their deductible and coinsurance; however, the HHS Office of Inspector General (OIG) is providing flexibility for healthcare providers to reduce or waive cost-sharing for telehealth visits paid by federal healthcare programs.
12. Q: How long does the telehealth waiver last?
A: The telehealth waiver will be effective until the PHE declared by the Secretary of HHS on January 31, 2020 ends.
13. Q: Can hospitals, nursing homes, home health agencies or other healthcare facilities bill for telehealth services?
A: Billing for Medicare telehealth services is limited to professionals. (Like other professional services, Critical Access Hospitals can report their telehealth services under CAH Method II). If a beneficiary is in a health care facility (even if the facility is not in a rural area or not in a health professional shortage area) and receives a service via telehealth, the health care facility would only be eligible to bill for the originating site facility fee, which is reported under HCPCS code Q3014. But the professional services can be paid for.
14. Q: Can qualified providers let their patients know that Medicare covers telehealth?
A: Yes. Qualified providers should inform their patients that services are available via telehealth.
15. Q: Should on-site visits conducted via video or through a window in the clinic suite be reported as telehealth services?
A: Services should only be reported as telehealth services when the individual physician or professional providing the telehealth service is not at the same location as the beneficiary.
16. Q: How is this different from virtual check-ins and e-visits?
A: A virtual check-in pays professionals for brief (5-10 min) communications that mitigate the need for an in-person visit, whereas a visit furnished via Medicare telehealth is treated the same as an in-person visit, and can be billed using the code for that service, using place of service 02 to indicate the service was performed via telehealth. An e-visit is when a beneficiary communicates with their doctors through online patient portals.
17. Q: Are the telehealth services only limited to services related to patients with COVID-19?
A: No. The statutory provision broadens telehealth flexibility without regard to the diagnosis of the patient. This is a critical point given the importance of social distancing and other strategies recommended to reduce the risk of COVID-19 transmission, since it will prevent vulnerable beneficiaries from unnecessarily entering a health care facility when their needs can be met remotely. For example, a beneficiary could use this to visit with their doctor before receiving another prescription refill. However, Medicare telehealth services, like all Medicare services, just be reasonable and necessary under section 1862(a) of the Act.
18. Q: Will CMS require specific modifiers to be applied to the existing codes?
A: CMS is not requiring additional or different modifiers associated with telehealth services furnished under these waivers. However, consistent with current rules, there are three scenarios where modifiers are required on Medicare telehealth claims.
- In cases when a telehealth service is furnished via asynchronous (store and forward) technology as part of a federal telemedicine demonstration project in Alaska and Hawaii, the GQ modifier is required.
- When a telehealth service is billed under CAH Method II, the GT modifier is required.
- Finally, when telehealth service is furnished for purposes of diagnosis and treatment of an acute stroke, the G0 modifier is required.
19. Q: What flexibilities are available in the Medicaid program to provide care via telehealth for individuals who are quarantined or self-isolated to limit risk of exposure?
A: States have broad flexibility to cover telehealth through Medicaid. No federal approval is needed for state Medicaid programs to reimburse providers for telehealth services in the same manner or at the same rate that states pay for face-to-face services. A state plan amendment would be necessary to accommodate any revisions to payment methodologies to account for telehealth costs.
For more information, click here.
Even more resources –
AMA’s COVID-19 Resource Center for Physicians.
AMA STEPS Forward Module on Telemedicine.
AMA Data File requests (CPT data file, etc.).
Texas Medical Association has created a significant suite of telemedicine resources.
The National Governors Association is tracking state activities related to COVID-19
For the latest information on federal policy and payment changes related to telehealth in the midst of COVID-19, visit the CMS Current Emergencies site.
American Psychiatric Association – General resource page & toolkit on COVID-19 and telepsychiatry
American Academy of Child & Adolescent Psychiatry – Telepsychiatry Toolkit
American Academy of Pediatrics resources on telemedicine.
American College of Physicians resources on COVID-19 and telemedicine